The Importance of Reporting Adverse Events
Written by Lucy Platt

During Med Safety Week, we reflect on the importance of reporting adverse events
Reporting adverse events is crucial in identifying potential safety issues and relevant risks in drug administration. An adverse event (AE) is any untoward occurrence that is experienced by a person following administration of a medicinal product or a medical intervention to that person. An adverse reaction is an AE that is suspected of being related to that product or intervention.
People are usually willing to report adverse drug reactions (ADRs) because they suspect a relationship between a medicine and the event. But it is important to report all AEs and not only limit these reports to ones we believe to be related.
Why do we need to report all AEs?
Reporting of all AEs, even if they are not perceived as particularly harmful and are not considered to be definitely related to the medicine, allows collection of a large amount of data for that product. There may be trends or patterns emerging from this dataset that can only be observed on a larger scale and are difficult to distinguish on an individual basis. For example, with enough well-documented reports one might determine the event to be a new ADR or interaction, or new information on a known ADR may be identified. The information gathered from the AE reports could provide information on interventions to treat these events. Alternatively, the information could help to support the current understanding of the known safety profile.
Why do we not report all AEs?
In a study by Johansen et. Al (2021), only 39.1% of adverse events in obstetric care in Norway were reported. Johansen et al suggested several reasons for under-reporting adverse events including shame and guilt or for fear of punishment. There could also be other reasons such as the feeling that AE reporting is less of a priority than all the other urgent tasks for busy healthcare professionals, the difficulty or ease of reporting in that particular region, or reluctance borne out of the belief that this report will not make a difference overall. There could also be a belief that reporting an AE will somehow lead to legal action. The ‘reporting culture’ differs between clinical environments and different countries.
What happens to the AE reports?
When an AE or ADR report is received by a regulatory agency or manufacturer of the medicine it is entered into a safety database. The name and contact details of the patient are not entered so that only the details of the event and any other information that is relevant to the assessment of the event will be stored.
There are sophisticated algorithms used by global pharmaceutical companies and regulatory agencies around the world to detect “signals” (suggestions of new ADRs or new information on existing ADRs). If a signal is detected this is reviewed by specialists called pharmacovigilance scientists and medics to understand it further. Finding sufficient information to support a causal relationship they will update the product information leaflet to inform future patients of the possible risks. If there is adequate information in those reports it may even be possible to suggest ways to minimise the risk of developing that AE or ways to treat it. This is vital information to help improve patient safety.
How to report an AE:
In some countries there is an established reporting system to send the AE directly to the regulatory agency. However, all manufacturers must have a medical information department who will provide a telephone number for you to call and report AEs directly to them any time of the day. If you search online you can find this number and let the medical information team know the details of the event. If you don’t wish to do this you can report the AE to your pharmacist or to any healthcare professional you are seen by and ask them to report it for you, but this is not guaranteed.
What information should I report?
There are some pieces of information that are really helpful when assessing these reports. These include:
Medication: name, dose and any other details of the medication (e.g. formulation such as tablet/syrup etc).
Timing: when did you start the medicine and when did the AE begin?
Medical conditions: why did you take the medicine? Any other conditions you suffer from.
Concomitant medications: any other medicines or herbal remedies that you were taking at the time of the event (including those you bought over the counter). If you stopped taking a regular medication just before the event began it is important to mention this.
Event: what happened? Providing as much detail as possible will really help in assessing the report, particularly any hospitalisation or treatments.
Dechallenge: what happened when you stopped taking the medicine? Did the AE resolve?
Rechallenge: did you start taking the medicine again? If so did the AE recur?
Anything else: if you think there is something relevant that is not in the above list (e.g. the event happened just after going to the gym or painting the fence) it is important to mention it.
Every AE report can make a difference. If you need to report an AE, find information on how to do so here
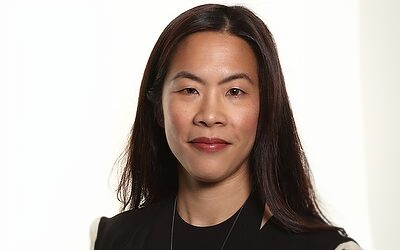
Conversations with Industry Leaders: Dr Sue Lim 1 April 2025
By Dr Stephanie-Jayne Jones
On 1st April I caught up with Dr Sue Lim in the latest in my series of “Conversations with Leaders in our Industry”. Dr Lim is an experienced former FDA director and licensed physician with around 2 decades of global drug development experience.
Conversation with Industry Leaders: Professor Alan Boyd 11 April 2025
Continuing my (Dr Jones’) series of conversations with leaders in our industry, I caught up with Professor Alan Boyd before Easter. Some of you will know him as the former President of the Faculty of Pharmaceutical Medicine, some will know him as the entrepreneur who created @Boyds and others will know him as an engaging and expert mentor, dedicated to training and empowering the next generation of people working in the pharmaceutical industry.
Understanding Gaucher Disease
Gaucher disease is a rare genetic disorder caused by a deficiency in the enzyme glucocerebrosidase, leading to a harmful buildup of fat in cells. This causes symptoms like enlarged organs, bone pain, and, in some cases, neurological impairment. Current treatments offer relief but come with limitations such as inconvenient infusions, side effects, and the inability to address neurological symptoms. Read on to discover the promising new developments bringing hope for this rare disease…