By Dr Steph Jones 
World Cervical Screening Awareness Week started on the 17th of June and this year it runs until my birthday, 23rd June. Cervical cancer is one of the few types of cancer where there is a screening tool available in many countries, that allows us to detect it early, increasing the chance of a cure. There are also immunisations that can reduce the risk of developing this type of cancer. I’m really pleased that these have become part of the childhood immunization programme in many countries now, protecting generations of our children to come.
However, despite these advances, cervical cancer continues to affect a lot of people around the world, being the 4th most common cancer in women and 9th most lethal cancer worldwide. Some of this is due to people not knowing enough about cervical screening and the benefits of immunization, such as a patient whose story has stayed with me since medical school (see later). To embrace this awareness week I’m sharing some facts about cervical screening. (These are based on the current UK NHS cervical screening programme, therefore check your local cancer screening services for more information outside the UK).
Where and what is the cervix?
For people with a uterus (womb) the cervix is the neck of the uterus, at the top of the vagina. Most cervical cancer starts in the transitional zone, where it becomes the entrance to the uterus. This is why the sample is taken from this area during cervical screening. Most cervical cancers are caused by specific types of human papilloma virus (HPV). 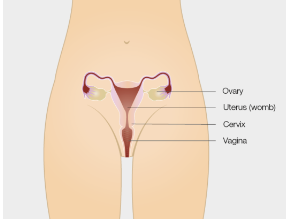
How is the sample taken?
The test involves using a soft brush to take a small sample of cells from the surface of the cervix. The brush has a long handle and will be inserted by someone who is trained to take these samples. To make this more accurate they will first make sure the person is comfortably lying on their back, and gently insert a device called a speculum, which allows them to see the cervix clearly. Having had many of these myself over the years I can tell you that although it is not very dignified and there can be some slight discomfort (like pressure) during the procedure, it is over very quickly and the people taking these samples are understanding and will try to help you relax. They will offer you a chaperone if you need someone with you while it is happening.
How is the sample analysed?
The sample is put into a small plastic container and sent to a laboratory. It is generally first tested for the types of HPV that have the highest risk of causing cervical cancer. If there is a negative result for the high risk types of HPV, the risk of cervical cancer is very low and there is no need to check for abnormal cells (even if the person has had these in the past). (In the old days the sample was “smeared” onto glass to be looked at under a microscope, so you may have heard the expression “smear test”).
If there is a positive result for HPV the sample is then also checked for abnormal cells. Abnormal cells are not cancer, but they could develop into cancer if left untreated.
What happens if there are abnormal cells?
The next step may be to offer another examination called a colposcopy. This is a similar procedure to the cervical screening test, but involves a camera to look at the cervix more closely. During colposcopy the abnormal cells could be removed.
This is how screening can prevent cervical cancer.
Does it work 100%?
Unfortunately, immunization and screening does not always prevent people from developing cervical cancer. In some cases this is because the cancer develops in the years before, after or between screenings, or the screening test did not detect an issue (possibly due to a rare type of HPV or because the abnormal cells were not picked up in the sample). This could mean the cancer could be too difficult to treat by the time it is detected and therefore can’t be cured completely.
If the person does not attend for cervical screening when they are invited, the cancer can grow and spread for many years without causing obvious symptoms until it is too late to cure.
Patient story
One of the patients I met during medical school had “Iatrophobia”, this means a fear of doctors. She did not understand what was involved in cervical screening and was too afraid to attend her cervical screening tests. Unfortunately at that time the immunisations for HPV were not available so she had no way to protect herself from catching HPV and no way to monitor for cervical cancer, as she declined her invitations for screening.
Sadly for her she developed cervical cancer. At first she ignored the symptoms of post-menopausal bleeding and abdominal pains, until the blood loss became so severe she developed anaemia. She collapsed one day, due to the anaemia, and had to be admitted to hospital (her greatest fear!). By this time she had lost a lot of weight, and the cancer had spread to surrounding tissues. She then took up the offer of surgery, followed by chemotherapy, and underwent a massive operation to remove the uterus, cervix, and much of the surrounding tissues (Wertheim’s procedure).
This patient overcame her iatrophobia but was in hospital for many months and had years taken off her life. If she had attended for cervical screening for a few minutes every few years she may have been able to prevent this completely.
Signs and symptoms of cervical cancer
Monitoring is important to identify signs that could suggest potential cancer. These include:
- Bleeding between periods
- Bleeding during or after sex
- Bleeding at any time after menopause
- Unusual change in vaginal discharge
- New pain in the lower back, between the hip bones or lower stomach
- Rarer symptoms include leg swelling due to fluid accumulation in lymph nodes and painful urination or bowel movements, as well as loss of bowel and bladder control.
Although screening is in place for those most at risk of this cancer, there are several years between screening tests, and some people outside of the screening age group may be affected in rare cases. It is therefore important not to wait for the next screening test if you experience any symptoms, but to seek medical advice as soon as possible.
If you have been offered a screening test, don’t delay, book it today.
References:
https://www.gov.uk/government/publications/cervical-screening-description-in-brief/cervical-screening-helping-you-decide–2
Cervical cancer (who.int)
Cervical screening: programme overview – GOV.UK (www.gov.uk)
Cervical cancer risk | Cancer Research UK
Information on the HPV vaccination from September 2023 – GOV.UK (www.gov.uk)
Click here to go to Pharmora’s Home Page